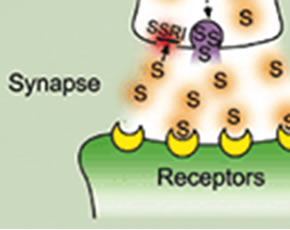
Limited data have suggested that the selective-serotonin reuptake inhibitors (SSRIs) may have anti-inflammatory properties in addition to their antidepressant effects. Here, Sacre et al (Arthritis Rheum 2010; 62(43): 683) explore the mechanisms of two SSRIs (fluoxetine and citalopram) in models of experimental arthritis.
Methods
Inflammation was induced in the paws of male DBA/1 mice by immunizing with type II collagen and adjuvant (i.e. the collagen induced arthritis model of inflammatory arthritis). Thereafter, mice were treated with either fluoxetine, citalopram, or an inert vehicle. Clinical characteristics of the mice, immunoglobulin levels, inflammatory cytokines, and articular histology were compared between groups. Next, the ex vivo effect of increasing concentrations of fluoxetine and citalopram on cytokine profiles and signaling through Toll-like receptors (TLRs) in murine marrow-derived macrophages and in cultured human macrophages and synoviocytes.
Results
There was a dose dependent decrease in quantitative measures of disease activity, paw swelling, histologic evidence of inflammation and erosive damage, and serum IL-12 with increasing doses of fluoxetine. Fluoxetine did not affect serum anti-collagen antibody levels. Effects were similar, but to a lesser magnitude, in citalopram treated mice.
In murine marrow-derived macrophages, both fluoxetine and citalopram inhibited cytokine production induced by TLRs 3,7, and 9 (but not TLR4) in a dose-dependent manner. In human cultured macrophages, both fluoxetine and citalopram inhibited activation of TLRs 3 and 8. In human synovial membrane cultures, both fluoxetine and citalopram inhibited the spontaneous production of TNF and IL-6, an effect that was not due to the effects of increasing serotonin or reduced cellular viability.
Conclusions
Fluoxetine and citalopram reduced the signs of murine inflammatory arthritis, reduced TLR induced cytokine production in murine marrow-derived macrophages, and reduced cytokine production in human macrophages and synovium culture ex vivo.
Editorial Comment
These results are interesting, and support a potential mechanism whereby SSRIs may play a role in ameliorating inflammatory arthritis. However, there are no human data regarding their short or long term ability to reduce inflammation, modify synovitis, or abrogate erosive articular damage. Thus, there are many more research steps required to support the use of this class of drugs in humans with inflammatory arthritis.

