Tumor necrosis factor-α (TNF-α) inhibitors have revolutionized the treatment of rheumatoid arthritis (RA). There are currently three TNF agents on the market for RA; among these, infliximab is a chimeric monoclonal antibody against TNF-α administered as an infusion. Golimumab is similar to infliximab, except that it has been engineered to be fully human and is given as a subcutaneous injection. Here, Kay et al (Arthritis Rheum 2008; 58: 964) report the results of a randomized, double-blind, placebo-controlled, phase II dose-finding and safety study of golimumab in patients with active RA.
Methods
Patients with active RA who were receiving at least 10 mg of methotrexate per week were randomized to one of five groups:
- Blinded placebo for 20 weeks, then open label infliximab at standard dosing through 44 weeks
- Golimumab 50 mg every 2 weeks for 20 weeks, then every 4 weeks through week 48
- Golimumab 100 mg every 2 weeks for 20 weeks, then every 4 weeks through week 48
- Golimumab 50 mg every 4 weeks through week 48
- Golimumab 100mg every 4 weeks through week 48
The primary study endpoint was the ACR20 response at week 16. Secondary outcomes were change in DAS28 and ACR-N at week 16, and ACR20, 50, and 70 responses at week 52. Safety, pharmacokinetic data, and induction of anti-golimumab antibodies were monitored throughout.
Results
One-hundred seventy-two RA patients (34-35 per group) were randomized. The majority of patients were women (77%) with a median age of 54 years. Median baseline DAS28 (CRP) was 5.2 and the median baseline HAQ was 1.6. Although there were no statistically significant differences between baseline characteristics between the combined golimumab groups and placebo, there were heterogeneities within the individual golimumab dosing groups. At 16 weeks, 83% of patients in the placebo group remained in the study compared to 88% of those in the combined golimumab groups. By week 52, 60% of patients in the placebo group remained compared to 79% in the combined golimumab groups (p=0.02).
| Table. Efficacy Outcomes at 16 weeks | |||
|
Placebo n = 35 |
Combined Golimumab groups |
p |
|
| ACR20 |
37.1 % |
61.3 % |
0.01 |
| ACR50 |
5.7 % |
30.7 % |
0.003 |
| ACR70 |
0 % |
12.4 % |
0.028 |
| ACR-N; median (IQR) |
0 (-12.5, 28.6) |
33.3 (0, 54.4) |
0.001 |
| Change in DAS28-CRP; median (IQR) |
-1.0 (-1.8, -0.2) |
-1.7 (-2.5, -1.0) |
0.002 |
| DAS remission |
5.7 % |
26.3 % |
0.009 |
At 16 weeks, combined golimumab responses tended to be superior to placebo (Table) with no statistical difference in response rate between the dosing groups. Steady state golimumab levels were generally attained by 12 weeks. Antibodies to golimumab were observed in 6.5% of golimumab treated patients and did not correlate to injection site reactions, changes in trough golimumab levels, or lack of efficacy.
Among non-serious adverse events, nausea was higher in the golimumab group compared to placebo (16.8% vs. 2.9%, respectively) and was increased in a dose dependent manner. There was no statistical difference in injection site reaction or the number of patients who discontinued the study due to an adverse event, although injection site reactions were highest in patients receiving the highest dose of golimumab. Serious adverse events, including serious infections, were observed in equal proportions between the active treatment and placebo groups. Among serious infections, 3 were seen in the placebo group (one each of lower respiratory tract infection, Listeria sepsis, and enterocolitis), the later two occurred in the phase in which placebo treated patients received open-label infliximab and both occurred in a single participant. Among the active treatment groups, 4 serious infections were observed through week 52, including 3 cases of pneumonia (H. influenza, S. pneumoniae, Legionella) and one case of septic shock. No treatment related deaths occurred during the study. Elevated LFTs were observed more frequently in the golimumab group compared to the placebo group.
Conclusions
Golimumab in addition to background methotrexate is more efficacious than placebo in patients with active RA. Serious adverse events were not associated with treatment.
Editorial Comment
Although the efficacy of golimumab was not tested against other TNF inhibitors in this study, its efficacy is unlikely to be superior other TNF inhibitors. Thus, the appeal of golimumab in an already crowded arena is primarily focused around marketing, as an injectible, fully humanized molecule with a potential injection frequency of monthly may be appealing to some patients. Although this study does not indicate an increased risk for infection with golimumab, the small numbers of patients involved and the limited follow-up time mean that definitive conclusions about safety remain to be answered. In particular, the avidity of golimumab for TNF-α and the longer half-life of the drug make infectious and other complications related to TNF blockade a greater theoretical risk that will require more research to determine whether these translate to more clinical events.
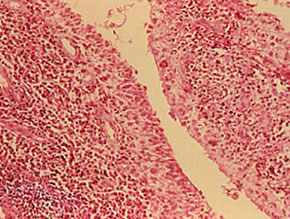
Figure: Reprinted from the Clinical Slide Collection on the Rheumatic Diseases, copyright 1991, 1995, 1997. Used by permission of the American College of Rheumatology.

